Print Shop
Dots and Lines of 3-D Bioprinters Help UVA Scientists, Step by Tiny Step
Tracking information showed the package had left Switzerland, arrived at an airport in Washington, D.C., then made its way to Charlottesville.
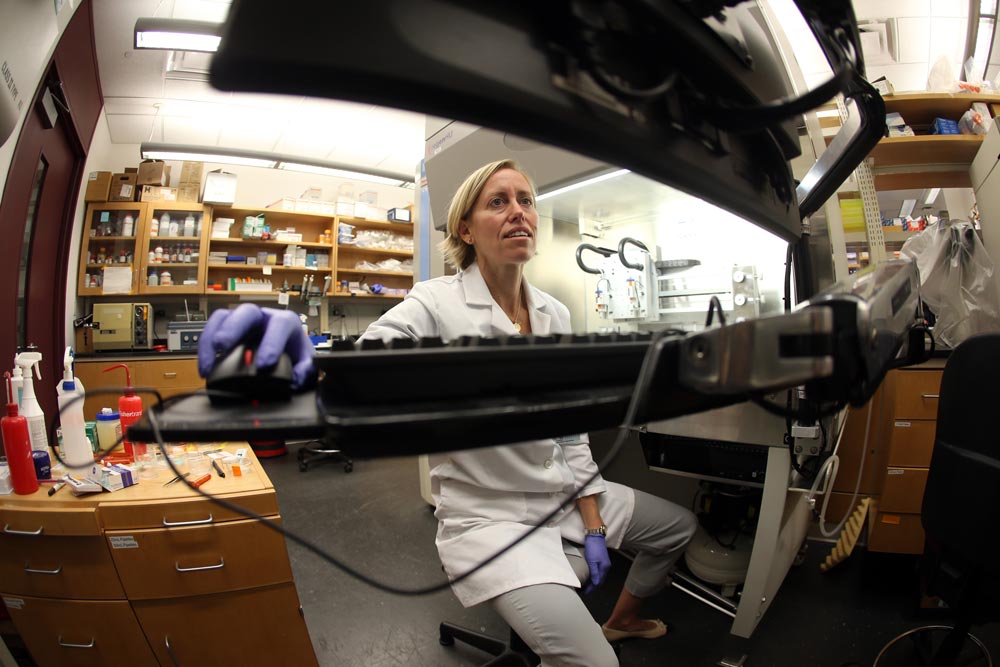
University officials watched it each step of the way. Inside was a pair of 3-D bioprinters, the kind that Shayn Peirce-Cottler, a bioengineering professor, had dreamed about for nearly a decade.
This was, in the most optimistic sense, the edge of the cutting edge, the very start to a start to a new reality. In a best-case scenario, it was the type of delivery that could change the landscape of organ transplant and personalized health for generations.
The regenHu 3DDiscovery is a three-dimensional bioprinter made in Switzerland with the kind of precision and design that give Swiss engineering its good name. A year earlier, the printer’s price tag had run close to $300,000—and engineers had access to only two in the nation. Now, because of a price drop, the University of Virginia could get two of its own for that price: one for Peirce-Cottler’s bioengineering lab and one in Kenneth Brayman’s lab in the Medical School.
Bioprinting is a relatively new technology, about 10 years old, and the University already owns an older bioprinter. But the 3DDiscovery is among the most precise and advanced of the printers, which allows for greater innovation.
Several UVA professors, including Peirce-Cottler (Engr ’02) and Brayman, a transplant surgeon, applied for a grant for the printer in February 2014, won approval for funding from the Office of the Vice President for Research at the University, then ordered the printers in February 2015.
When they reached Grounds in May, University officials had to wait for an engineer from Switzerland to fly over and assemble them.
“I was elated,” Peirce-Cottler says. And then, “I was a little scared.”
For years, biomedical engineers have struggled to build facsimiles of realistic human tissue. Those troubles are related largely to the construction of the tissues and maneuvering living cells. Or, as Brayman describes it, “putting the right materials in the right order.” The major barrier comes when stacking cells on top of each other, even two or three deep. Within hours, the first layer of cells can die.
With realistic facsimiles of human tissues, scientists believe, they could eventually “print” artificial organs, with which they could solve a host of health problems, such as heart, liver or kidney failure. With a bioprinter, scientists could add a level of precision that would eventually make the tissue more like human tissue. This, Peirce-Cottler says, could lead to a nearly complete rethinking of many current medical procedures and practices.
But every giant scientific breakthrough comes on the back of small, incremental successes that took place years earlier. So first, Peirce-Cottler and her team needed to understand exactly how this finely tuned instrument worked.
They loaded the printer with Nivea hand cream.
HERE’S HOW 3-D PRINTERS OPERATE: Instead of the ink used in traditional printers, these oversized machines “print” or “draw” using common manufacturing materials, such as titanium for satellite components, metals to build jewelry or plastics to mass-produce toys. Those materials are essentially squeezed out through a fine-point needle and placed onto a surface using design software that acts as a map, guiding the needle where to release the material and with what amount of pressure. The printer jots across the work area, adding successive layers of material.

Broadly, these 3-D printers are on the leading edge of technologies in hundreds of sectors; as a result, they are becoming more commonplace and available to everyday tinkerers, not just those in high-end research labs.
Bioprinters work much the same way. The UVA labs are using a variety of materials to print small objects as a way to familiarize themselves with the printers’ capabilities. The first attempts with hand cream looked like a freshly printed pattern on glue. But after the printer added layer upon layer, each project took shape.
“It’s beautiful to watch it work,” says Peirce-Cottler.
One of the first items her team made was a replica of the Rotunda.
They constructed Thomas Jefferson’s trademark dome—about an inch tall and an inch wide—from a product best known for preventing rough, dry skin. Hand cream is an ideal introductory material for the printer because it matches the viscosity and the soft squishiness of human tissue. The final product looked as if it were melting from the summer heat, but it stood nonetheless. A victory.
In another experiment, the team tried to build a simple cylinder, again about an inch in diameter. But in each iteration, as layers of hand cream were added, the structure collapsed in on itself and toppled over. A setback.
A team in the lab eventually figured out that the problem was the chemical and biological makeup of the hand cream. The ingredients are not perfectly blended, and as a result leave almost undetectable pockets of air and an inconsistent texture. After the printer placed each layer of hand cream on top of the last, some of the material seeped into the previous layer, causing the collapse.
On the next pass, the team tweaked the design to leave less spacing between layers. The difference was a fraction of a millimeter. The cylinder stood. A small victory and a baby step forward.
The lab’s next test was to print using collagen. It’s what is known as an extracellular matrix, a collection of molecules that are secreted by human cells. Peirce-Cottler describes the matrix as a kind of highway or carpet for the cells to “walk” along but also to communicate. Surgeons often remove excess collagen during medical procedures, such as routine hip replacement surgeries; UVA’s engineers then use it for research.
The team experimented by creating series of lines and patterns of dots. It was the kind of thing that might look like a test page for a printer, and yet another task that may seem routine. But Peirce-Cottler says the lines mimic muscle fibers and the dots are islets, or small clusters of cells, expertly placed to leave enough room for blood vessels. Another small victory.
Through a collaboration with plastic surgeons, the lab has also worked with human stem cells that are removed as part of liposuction procedures. The lab kept the cells alive in an incubator and then loaded them into the printer in a gel of nutrients, proteins and sugars that keep the cells “happy.”
Those cells are less controversial than embryonic stem cells. But while embryonic cells can divide and make themselves into different kinds of human cells again and again, these stem cells can divide only about 20 times.
The lab’s results were, by all practical definitions, extremely thin versions of living tissue. But in thicker versions of the tissue—anything over 100 microns, or 1.5 layers—cells begin to die within hours.
This is the next hurdle.
“None of this is going to work without blood vessel growth,” Peirce-Cottler says. Without oxygen, the cells starve for nutrients and die. This is where her expertise comes in: She studies microvasculature, a complex network of highly specialized blood vessels. And this is why the printer’s precision and improved design software take on such great importance.
The blood vessels need to be within a distance of 100 microns from the cell, or about 1 percent of the thickness of a penny. One of the printer’s key characteristics is that it will allow the lab to draw blood vessels directly onto the tissue with an astonishing level of precision.
Scientists already know how to grow blood vessels in the body, how to control them, how to stop them from growing and how to enhance them. “Cells know how to do everything,” Brayman says. “You just need to provide the right environment.”
In other words, they have a mind of their own. In fact, the stem cells begin to build blood vessels on their own from collagen; however, since they’re outside a familiar body, the tubing they’re building is essentially faulty or leaky plumbing. They have to be fooled into building good plumbing outside the body.
The challenge then becomes printing tissues that can create functioning blood vessels.
For example, with advancements in cell culturing technologies, the bioprinter could use someone’s own cells to help create or replicate organs, reducing the risk of rejection. Each day, 21 people who are on waiting lists for organ transplants in the United States die. In 20 to 25 years, Peirce-Cottler and Brayman hope, the bioprinter will play a key role in alleviating organ shortages.
Instead of making models out of hand cream, scientists hope bioprinters eventually can build an organ using a person’s own lab-grown cells. Throughout the nation, other bioengineers are working on producing transplantable ears, bone and muscle, sometimes using artificial materials and nonhuman cells, such as cow or pig cells, as the primary material.
The two labs work together closely, but Brayman’s lab focuses more on technologies that could be implanted directly into people, while Peirce-Cottler focuses on projects that would start with animals. If the UVA teams can advance the capability for blood vessels, in theory, the printer can solve a host of health problems.
But first there will be more immediate, incremental discoveries.
For example, Peirce-Cottler hopes that within about a decade doctors could load pancreatic cells into the printer, draw them into islets following a blueprint, and implant them beneath the skin of diabetics to produce the insulin their bodies demand.
In addition, the organs could test the safety of experimental drugs and help measure their effectiveness.
ALL OF THIS RAISES A QUESTION. The future for bioprinters and related health care technologies can seem dazzling. But is it a little too close to science fiction? The new capabilities bring with them underlying concerns about the ethics of regenerative medicine.

Mary Faith Marshall is a bioethics professor in UVA’s School of Medicine; her work includes studying the allocation of scarce resources. While she does not envision any new ethical arguments emerging from the printers, she suggests that the printers may provide a new twist on existing arguments.
“Many of the issues are the same as in other emerging technologies in health science,” she says. This includes questions of distributive justice, such as who will and won’t have access to printed organs and what happens when demand outstrips supply.
Specifically, she points to questions about regulations. While organ transplants certainly would be regulated by the federal government in the United States, how would other countries behave? She points to the potential for abuse for monetary gain and a lack of quality control. Will patients who lack the resources take unnecessary risks for a chance to receive an organ?
But Marshall is also optimistic about the technology and agrees that bioprinters could dramatically change some aspects of health care. As a result, these changes also would help solve—or at least diminish—many longstanding ethical conundrums.
For example, the printing of organs could mean less testing of new drugs and therapies on animals, which she calls a “good thing.” It could lead to more testing of these therapies and vaccines on cells in labs, and away from using other human organs. “It brings the possibility of great improvement,” she says.
ONE OF THE UNIVERSITY’S GOALS in purchasing the printers was increased collaboration across several disciplines. That has already happened. Peirce-Cottler’s and Brayman’s labs meet every other week to discuss their progress. They’re also working on projects with the department of orthopedics and the department of surgery.
University officials are planning a symposium on bioprinting for the spring to help share work within the regional bioengineering community.
Peirce-Cottler has stressed that the long-term benefits will require time and incremental improvement. It will mean more dots, more lines, more hard thinking about the backbone of science.
“It sounds like science fiction,” Brayman says. “But these are solvable problems.”
